For the last year ( two, if you count the pre–reqs) this has been my life, day and night. Some days I was sure someone glued me to the chair. Rose still asked everyday, “do you have studying, mom?” always hoping the answer might be no! I loved it though, I love school, (I know, I’m a nerd; the science was always my favorite part). I even liked taking tests, I like the feeling when I read a question and absolutely know the answer and can explain why, it is a powerful feeling. Then we got to work in the hospital with actual patients, and I was sure I was doing the right thing. I was scared out of my shoes that I wouldn’t know what to do, and often, I didn’t, but the patients always looked to me for help and comfort, and somehow I provided. I went from feeling like and impostor in white scrubs, grateful to be able to empty th e bedpan; to gradually being able to manage 3 patients care by myself and having the sense that they are “my” patients by the end of my preceptorship.
e bedpan; to gradually being able to manage 3 patients care by myself and having the sense that they are “my” patients by the end of my preceptorship.
Then we graduated a week before classes were over. We still had tests, and shifts, but we walked with our robes and hats and all. It felt great! That’s me in the middle of my new friends. Twenty nine years since my last graduation, this one meant so much, and I appreciated the opportunity so much more this time.
We did a few more presentations, and papers and exams, and then school really was over. We had our pinning ceremony, where we get pinned by another RN as a way of welcoming us into the profession. It was very touching, and we celebrated being done, finally!
 Here is my pin, the initials are for Samuel Merritt University, we are the first class to graduate from the University, after 100 years of being a College. That is a lot of nurses! It is inspiring to come from such a long tradition, too bad we didn’t get the little white caps too!
Here is my pin, the initials are for Samuel Merritt University, we are the first class to graduate from the University, after 100 years of being a College. That is a lot of nurses! It is inspiring to come from such a long tradition, too bad we didn’t get the little white caps too!
BUT…. the studying wasn’t really over yet. I still had to take the board exam, the NCLEX. So my friend Marti and I kept meeting everyday to study for a couple of hours. We practiced thousands of questions, and quizzed each other, and looked up obscure drugs and diseases. We even spent a couple of days in Tahoe with two other classmates to study away from the distractions of house and family. We really did study, though nobody believes us.  Then I spent a day in Yosemite, by myself, hiking and enjoying the scenery before I drove to Fresno to take my test.
Then I spent a day in Yosemite, by myself, hiking and enjoying the scenery before I drove to Fresno to take my test.
I couldn’t have been more ready for this test, we studied all year, reviewed for several weeks, I relaxed for a whole day, got a good night’s sleep the night before, ate a healthy salmon (brain food) lunch and had a latte, and walked into the test center ready to conquer it.
It was the wierdest test I have ever taken. First, they take you one at a time, after you have been photographed, fingerprinted and pockets emptied into the test room. They don’t even let you take a tissue in there, I had to leave my bottle of water and my dark chocolates in a locker outside ( those of you who know me, I always have a couple of dark chocolates on my desk with me when I take a test, for that little boost when my brain wears out!). They sit you down in front of the computer and log you in and let you know that you are being video and audio taped during the test and if you need a break, raise your hand and the proctor will escort you to the bathroom. So, I sit down, a little unnerved by all the security, but ready to get this done. I speed through the little tutorial that takes you through some sample questions and push the button to start the real test. Now I should tell you that we have six hours to answer from 75-265 questions with breaks scheduled at 2 and 3.5 hours. The test is constantly evaluating how you answer each question to determine what the next question will be. It keeps asking questions until it determines that you clearly pass or clearly fail. I was determined to go slowly and carefully read each question a few times, since you can’t go back and change your answers. The first few questions were pretty reasonable and I felt pretty sure I was getting them right, then boom, they got hard, drugs I had never heard of, questions about priorities that I couldn’t rank, and then phwew, a few math questions. I love the math questions, because I know how to do them, they are concrete. It is the question about which patient you would see first that always gets me. Well, I am tooling along, I don’t really keep track of how many questions I am answering, (the last time I looked at the counter, I was on 55). The questions are hard, and I feel like I am guessing on many. I am sure I am not getting most of them right, so I am shocked when the whole computer screen goes black. Oh NO!, there is a power outage! right in the middle of my test! will I have to start over? But no the proctor comes in to escort me out and I realize that the screen went black because I was done! I quickly tell her this can’t be, I am not finished yet, I haven’t answered enough questions! there is no way I am up to 75 yet. Can she check? She smiles and shakes her head, no, there has not been a malfunction and there is no way for her to check the number of questions I answered. In a daze I walk out, put my finger on the fingerprint checker (what, was I going to somehow sneak someone else in to take my place while being videotaped? it is really me walking out now!) I collect my stuff, and see that only and hour and ten minutes have passed since my test started. Well maybe I started a little bit early, since I arrived at the center early, let’s say and hour and 15 minutes. Still that is 75 questions in 75 minutes, there is no way, I was going to go slowly! what happened? Oh no! what if I went so fast that I answered most of the questions wrong and I actually failed! I get in the car to drive the 3 hours home and try to think of who I can call that will make me feel better. Marti; she took the test the day before me and we hadn’t talked yet. Aachhh, I hear the sinking silence on the other end of the phone when I tell her that it took me 75 minutes, she took 2 and a half hours with 2 breaks. I didn’t even get a break. That is bad news, Marti is the speedy smart one. When we studied together she usually had the answer before me. I made some more phone calls looking for reassurance, which was given but I didn’t feel it. Nothing was going to make me feel relieved.
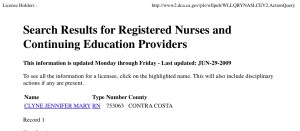
It has been 3 days now and I check the BRN website way to often to be considered sane, and still haven’t seen my name on the list of licensed RNs yet. I did the trick that someone said to try to register to retake the test and if the website won’t let you, then you passed. It wouldn’t let me, but I still don’t feel relieved. SO I AM STILL WAITING! I spent today listing all the hospitals that are within a one day drive of me and checking the job openings on their websites. The job hunt is another story that I will save for another post. In the meantime I am trying to keep busy and WAIT.








 Then I spent a day in Yosemite, by myself, hiking and enjoying the scenery before I drove to Fresno to take my test.
Then I spent a day in Yosemite, by myself, hiking and enjoying the scenery before I drove to Fresno to take my test.

